Turn and face the strange
With its upcoming ten year plan, the government is promising to unleash the power of innovation in an English NHS which has often seemed slow to adapt to new realities and adopt new technologies. Craig Ryan talks to innovators and experts about what needs to change about the way we change.
In 2023, the King’s Fund ran a series of workshops for 100 innovators working in health and care, where they shared their experiences of trying to transform services in a system under severe pressure. Reflecting on the sessions, the Fund’s digital technologies lead, Pritesh Mistry, wrote: “We noticed how quickly, and how often, frustrations bubbled to the surface. Our discussions would quickly turn from what is possible to the reality of how hard it is to innovate in the NHS and social care.”
The think tank’s report on the workshops describes innovators as “siloed”, “unsupported” and “hindered” in a service where “there is no space to do things differently”. It’s no surprise, the report concludes, “that innovation happens in pockets and that the NHS and social care have a reputation of being slow to innovate”.
In January, health secretary Wes Streeting promised his eagerly-awaited ten year plan will “empower NHS leaders to deliver the innovation and reform required to fix the NHS”. Like a lot of criticisms of the NHS, the claim that it’s hostile to innovation has a whiff of truth, but exaggeration and repetition has turned it into an unhelpful cliché. Everyone’s clear that something has to change about the way the NHS does change, but a lot less clear about what needs fixing and how it’s going to get fixed.
Fantastic launchpad
“I would push back against the idea that the NHS is culturally hostile to innovation,” says Tim Horton, the Health Foundation’s assistant director of insight and analysis. “The NHS has been the birthplace of many celebrated innovations – MRI scanning, CT scans, hip replacements and ocular lens implants, to name a few. We see NHS teams coming forward with great ideas all the time. Instead, I’d say the challenge lies in scaling innovation across the system.”
As our case studies here show, world-class innovation does happen in and around the NHS. But the experiences of most innovators we contacted tend to bear out the King’s Fund’s finding that “innovation happens, not because it is supported by the system but in spite of it, due to the energy and drive of enthusiastic individuals.”
-

It seemed like an obvious problem we needed to solve upstream.
Former GP Dr Bea Bakshi, CEO of C the Signs, explains how her pioneering AI-tool is helping GPs to spot the early signs of cancer.
Dr Ross Harper, a neuroscientist and chief executive of Limbic, which has developed the only AI-powered mental health tool licensed as a medical device in the UK, insists that NHS trusts can be a “fantastic launchpad” for tech innovation. “Technology is really great at alleviating the supply-demand problems NHS trusts face, so when they have autonomy over how they solve pressing issues, that’s a great test bed,” he says.
Mental health trusts like Surrey and Borders, Essex and Lincolnshire, which pioneered use of Limbic as a digital front door to services, “didn’t decide to use AI because it’s cool”, he says. “These really passionate, heart-in-the-right-place NHS services took a gamble on Limbic because they believed we could help solve their problems.”
But — and you knew one was coming — “the NHS is a very difficult customer for any company that needs commercial viability”, Harper warns. Problems with scaling, funding and procurement could, he fears, lead to fledgling healthcare tech firms leaving the UK to grow up elsewhere. “They’re not problems with anyone working in the NHS; they’re system problems and they’re very real,” he says.
The fragmented NHS structure in England, with thousands of bodies potentially taking individual decisions on investment, transformation and procurement makes it hard to scale innovations even when they’ve proven effective.
“The challenge is that every ICB wants to run its own pilot rather than adopting proven innovations at scale. This slow diffusion curve makes NHS-wide adoption difficult,” explains Dr Bea Bakshi, who developed ‘C the Signs’, an AI-powered tool that helps GPs spot patients at risk of cancer..
She wants the NHS to put more resources into making sure that proven innovations like C the Signs are implemented effectively on the ground. “If GPs actually use it, cancer detection improves. If they don’t then it’s not a good investment for the NHS, ICBs or GP practices. Implementation science is key — not just innovation.”
Dr Rishi Das Gupta is chief executive of the South London Health Innovation Network, which supports innovators and NHS organisations working together to transform services. He says it’s much easier to scale innovation where services are standardised around a clearly-defined group of patients.
-

We still live in isolated silos.
Angie Doshani, consultant obstetrician at Leicester Hospitals on developing JanamApp, a new tool to support Asian women through pregnancy.
“If 80% of patients can benefit, I can expend the energy required to innovate and make the whole pathway better for those patients,” he explains. He gives the example of hybrid closed loop technology for treating diabetes: “It’s a good product, it actually changes lives. In one year we managed to get rollout to 70% of patients. It scaled really easily.”
The big challenge now, he says, is doing that for generalist services, like integrated neighbourhood teams, community care and GPs, where “the change might benefit only 5% of patients and I might unravel a lot of other things by innovating.”
Maddening and irrational
All our innovators and experts all agreed that the NHS framework for funding and supporting innovation needs an overhaul. “Money is released, but it goes into different pockets and budget holders are diffuse and obfuscated,” says Limbic’s Ross Harper. “Not even people within the system really know how to access that funding.”
He recalls being told recently by one very senior NHS leader that trusts with funding to expand capacity often can’t find new staff, but can’t spend the money on time-saving tech solutions instead because it has been ring-fenced for staff costs. “We were being very respectful, but it was a maddening, irrational conversation; both parties recognised it was counterproductive, yet there was nothing we could do,” Harper says.
Das Gupta reckons building a case for investing in innovation is harder in the UK than in any other major health system. “I can’t build a multi-year business case because I don’t have a multi-year financial settlement from the government,” he explains. NHS organisations are also not incentivised to grow through innovation, he says, because “the only benefit we can draw is the cost reduction. We don’t assign monetary value to patient experience, staff experience, or learning and innovating in itself. We keep it narrowly to financial savings and that makes it harder.”
He worries that this lack of return could encourage successful healthcare tech businesses to move abroad. The thing he most wants to see in the ten year plan is a change in the financial incentives “to allow organisations which innovate to retain some of the financial benefits that they generate for the system as a whole. That’s the big one,” he says.
-

We waste so much money trying to implement something that doesn’t work.
Rebecca Howard, founder of Shiny Mind, explains how the firm co-designed a digital mental health programme with NHS staff in Liverpool.
Sad story
Innovators also point to other ‘system’ barriers to innovation, including ponderous decision-making, labyrinthine procurement processes and a risk-averse culture that penalises failure while insufficiently rewarding success. Government adviser Paul Corrigan recently described the NHS as “a pretty bad partner” for tech firms, because it didn’t know what it wanted, bought what was offered rather than co-developing solutions, and took too long to approve contracts.
Professor Angie Doshani, consultant obstetrician at Leicester Hospitals, says rolling out JanamApp, a successful online tool she developed to support south Asian women through pregnancy has “been a challenge, not because people don’t love it — they do — but because every trust does procurement differently, and there’s no standard. When you you’ve cleared one hurdle, there’s another. That’s frustrating for me as an innovator.”
She would like to see a “national pathway” for innovation adoption, with trusts modifying their own approaches to meet the national standard. “That would make life easier for innovators and for trusts,” she says.
“It’s a sad story,” reflects Doshani — who still works in the NHS — that so many innovators feel they need to leave the NHS to develop their ideas to improve NHS services. “If the NHS wants to recognise innovation, they need to support the innovator,” she says. “Having something with NHS support makes spread and scale so much easier. If you’re already working in the NHS, why should you have to go outside and then try to get back inside?”
Innovators need “as much evidence as possible, even in the early days,” advises psychologist Rebecca Howard, founder of the digital mental health and wellbeing platform Shiny Mind, because the NHS requires a “huge level of certainty to move forward with an innovation.”
Co-design is key, she believes: too many innovations fail because they haven’t been developed and tested with patients and staff. “But because the NHS doorway isn’t particularly open or easy to access, innovators end up developing services without them being tested with the people that are going to use them,” she says.
The tough regulatory framework in the NHS may look like another hurdle, but Limbic’s Ross Harper says it can actually help innovators by weeding out the ineffective or quack solutions that damage trust. “Just deregulating doesn’t necessarily mean you’re going to see more innovation,” he warns.
Tighter rules on what can be classed as a medical device in mental health, recently introduced by the MHRA, will help innovators by “bringing clarity and establishing hard lines,” Harper says. “Innovation will be stifled far more by scandals and patient harm than regulation. I’m a huge advocate of AI in healthcare, but I’m terrified of an unregulated ecosystem allowing bad actors to have a go, cause a problem and set the field back.”
-

I haven’t come across as many barriers as you’d expect.
Anna Lisa Mills, sustainability manager at Newcastle Hospitals, explains how new technology is helping to decarbonise the NHS supply chain.
Valued priority
The Health Foundation’s Tim Horton urges the NHS to shift some innovation funding towards “capacity building” — giving staff the training and time they need to refine and successfully implement innovations. “In many cases, just a small amount of additional investment —whether that’s training, mentorship or change management resources — can make a huge difference,” he says.
“If we truly want to embed innovation within the NHS, we need to signal that it’s a valued priority,” Horton adds. “That means recognising and rewarding efforts to implement new ideas, even when they don’t immediately succeed.” And while a degree of pressure can be a spur to innovation, the day-to-day pressure on NHS services means “innovation tends to drop off because people simply don’t have the bandwidth to engage with new ways of working,” he warns.
Let’s end on a note of optimism: the ten year plan is an opportunity to make the NHS a great place for innovation. None of the problems we’ve heard about should be too big to tackle in what Keir Starmer has called the “biggest reimagining in the NHS since 1948”.
“While the NHS is a very difficult customer, it’s a nationally cohesive system with incredibly high-quality data reporting,” says Harper. “We have institutions like Cambridge, University College London and Imperial College, that bring the world’s best AI talent to the UK — where there’s an amazing pool of data to support innovation and a willing sandbox to deploy new solutions.
“That’s why I think the UK will be the launchpad for the most important healthcare AI company in the world. And the NHS will be a massive part of that,” he says. “The challenge now is to make sure that company stays in the UK and doesn’t commercialise somewhere else.” //
Related Stories
-
Co-production: say it like you mean it
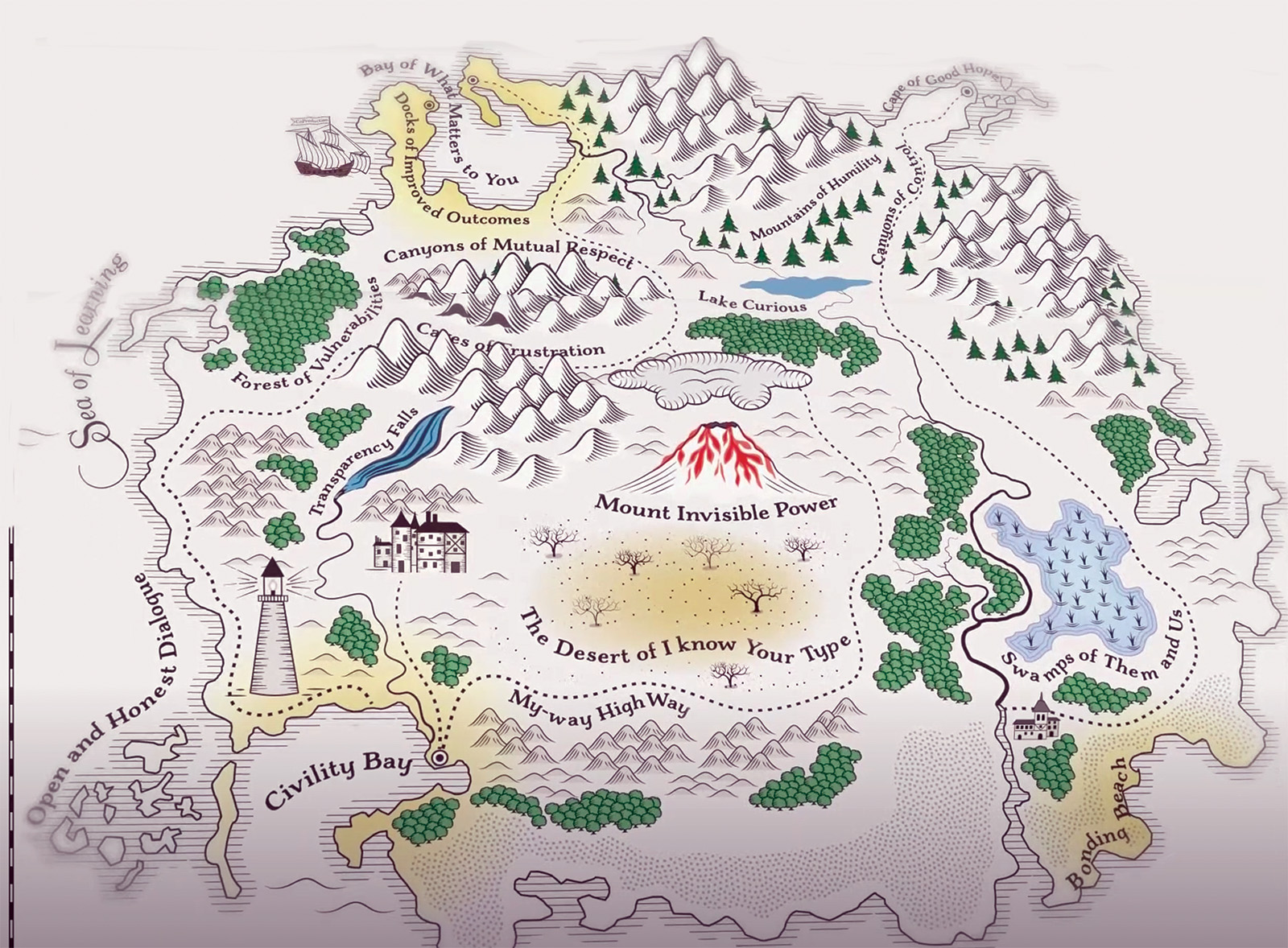
The NHS talks a good game on co-production, but many patients and carers still feel service changes are done ‘to’ them not ‘with’ them. As Jessica Bradley discovers, meaningful co-production means building lasting relationships and sharing decision making power.
-

Holyrood elections: Back from the brink—for more of the same?
After a big scare last year, the SNP are now clear favourites to extend their rule at Holyrood into a third decade, pointing to incremental reform rather than radical change for the NHS in Scotland. Rhys McKenzie reports.
-

Senedd elections: Tough choices, empty promises
As we enter 2026, the NHS in Wales faces some stark choices and a likely change of government. But the parties vying for power at Cardiff Bay will need to up their game to meet the challenges ahead. Craig Ryan reports.
Latest News
-

FDA General Secretary Election 2026
Please find important information regarding the FDA General Secretary Election 2026 which MiP members may participate in.
-

Government proposal for sub-inflation pay rise “not good enough”, says MiP
Pay rises for most NHS staff should be restricted to an “affordable” 2.5% next year to deliver improvements to NHS services and avoid “difficult” trade-offs, the UK government has said.
-

Unions refuse to back “grossly unfair” voluntary exit scheme for ICB and NHS England staff
NHS trade unions, including MiP, have refused to endorse NHS England’s national voluntary redundancy (VR) scheme, describing some aspects of the scheme as “grossly unfair” and warning of “potentially serious” tax implications.