Method to the madness? Six questions the ten year plan must answer
The NHS system in England has been blown up and thousands of managers are set to lose their jobs without knowing why, writes Craig Ryan. The upcoming ten year plan has a lot of questions to answer. Here are six of the biggest.
1. How do we do this?
Let’s take this first because it mustn’t be an afterthought. We don’t need another ‘compelling vision’ for the triple shift (to prevention, to community and to digital — in case you need reminding). We get it. We need to know how it’s going to happen.
Almost everyone I speak to, whether manager, clinician or system leader, is privately extremely sceptical that the triple shift—particularly out of hospitals—will happen. That’s not a good start. However good the vision is, it won’t get off the ground without a clear, credible plan for achieving it. What we’ve seen so far, in the blizzard of announcements, hints and deathbed edicts from NHS England, is as clear as mud.
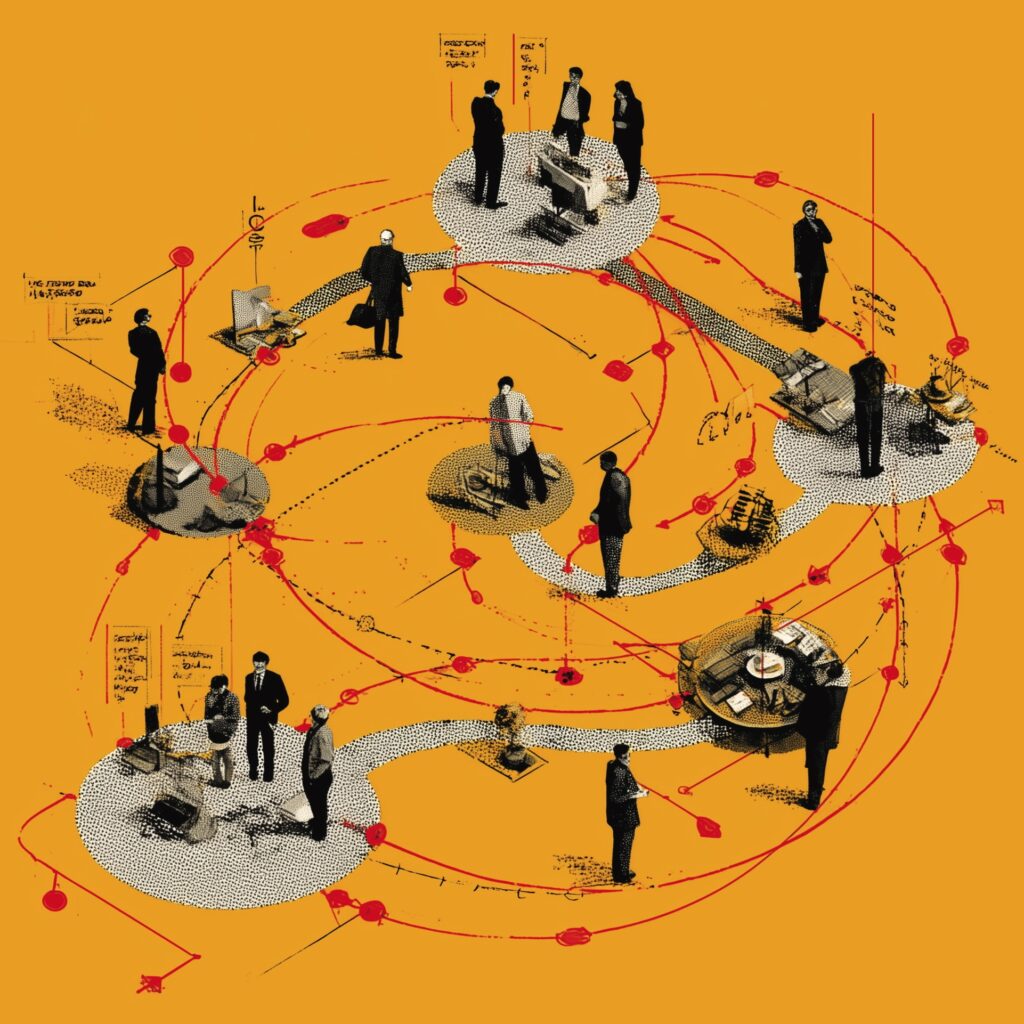
The plan “cannot simply describe policy changes; it must give an indication of how delivering this change will be possible”, says Sarah Walter, director of the NHS Confed’s ICS network. “Each part of the system needs to be clear on its purpose, what it is accountable for, and to whom, something that does not currently exist. Instead, historic structures are layered on top of one another like a coral reef.”
2. What are the trade offs?
The plan needs to include a brutally honest assessment of what can be done and when. Promising more of everything while hiding behind glib mantras like “we have to do more with less” isn’t good enough. We’ve been doing that for years.
The government has made the trade offs even harder by cutting NHS management off at the knees before it even starts. These are not small ‘administrative’ cuts, trimming off waste and duplication, they’re a step (down) change in the NHS’s capacity to reform itself.
The June spending review included a decent financial settlement for the NHS, but it won’t avoid the need for those ‘difficult choices’ that politicians like to talk about in theory but often duck in practice. If the 18-week elective care target is the key priority, what weight do we give to A&E waits, cancer standards, ambulance response times or mental health waiting lists?
“They must know that it’s not enough to achieve all the ambitions in their manifesto,” warns the King’s Fund’s policy director, Siva Anandaciva. “It’s only when we see the rest of the reform plans… that we will know what in our health and care service will be fixed, what can be patched, and what might — unfortunately for us all — stay broken.”
3. Is collaboration still the thing?
“Is collaboration out of fashion already?” asked the Health Foundation’s Phoebe Dunn in a recent blog: ICBs have been stripped of their role as “system convenors”, while regulators seem to be refocusing on individual organisations rather than systems. “There’s talk of new league tables,” she adds, and a new performance framework that “judges providers solely on their own merits”.
We really need to know, but ministers are facing both ways on this. Health secretary Wes Streeting and his colleagues still talk about collaboration, particularly in the context of the “neighbourhood NHS” and public health. But the mood music and the government’s reforms so far point in a different direction. Maybe all this recycled Alan Milburn stuff can be reconciled with collaborative working—it will be interesting to find out how.
If not, this will be a serious upsetting of the apple cart — and one that flies in the face of the evidence. As the King’s Fund’s Chris Naylor points out, the best performing systems have invested the most time and money into collaboration between health, care and other public services. “The challenges demand a systemic response,” he says. “Going backwards on the commitment to system working simply isn’t a viable option.”
4. How do we integrate?
Collaborative working is still counter-cultural in the NHS. It won’t happen just because Whitehall wants it or the ‘logic of the system’ seems to point that way. Maybe “the conditions were never right for ICBs to perform their role as system convenors”, says Naylor, but somebody still has to do it.
That could be beefed-up integrated care partnerships, like the one being modelled by Suffolk and North East Essex, or, as advocated by MiP chief executive Jon Restell, new statutory regional bodies “big enough to carry heft and consolidate resources, but small enough to take on locally sensitive functions”.
Another option is providers themselves. Trusts are already set to take over several strategic functions from ICBs, including local workforce planning, infrastructure and primary care reform. Recent comments by Streeting that he wants to see an end to distinctions between different types of trust (‘acutes’, ‘community’ and so on) may indicate the direction of the government’s thinking. Or not.
There are problems with this — not least that there’s a lot more to place-based working than providing treatment services — but it couldn’t be worse than trying to do it from the centre. “The government machine’s evident operational inadequacy over the last few months should put paid to any idea of managing the NHS from Whitehall, directly or via regional outposts,” warns Restell.

5. What will drive improvement and productivity?
Stalled productivity in the NHS over recent years is perhaps the biggest headache for politicians and system leaders alike. The ten year plan needs credible proposals to drive improvement, upskill staff and quickly roll out effective new technologies.
But the implication of the government’s reforms to date is that the main problem is too many managers and not enough ‘frontline’ clinical staff. That flies in the face of all evidence. Productivity has fallen despite big increases in clinical numbers since 2019 and research shows that organisations with more managers tend to perform better.
Any new performance regime needs to free managers to innovate and collaborate locally — just replacing the dead hand of NHS England with the blunt instrument of league tables won’t do. If ministers want to “reinvent” the foundation trust model with “even more freedoms”—as Streeting has suggested—they need to explain how such organisations will be motivated to co-operate rather than just look after themselves.
Setting clearer priorities and reforming targets, payment systems and regulation “will make limited difference without also supporting the NHS’s capacity to improve”, says Health Foundation innovation expert Penny Pereira.
The government needs to embrace evidence-based ‘improvement approaches’ so local leaders can “shape implementation and effectively engage staff,” Pereira explains. “The government’s health mission needs thousands of teams in hundreds of organisations to have the licence and means to do things differently.”
6. How will the NHS win back staff?
It’s not just the public who’ve lost faith in the NHS (see the latest British Social Attitudes survey)—it’s staff too. The NHS staff survey shows little improvement in morale and motivation since the pandemic, a loss of faith in team working and almost a third of staff feeling burnt out all the time. The infamous ‘loss of discretionary effort’ since 2020 may become permanent.
“The findings demonstrate that working in the health service continues to look like an unattractive career, with many NHS staff feeling undervalued and overstretched,” warned King’s Fund director of leadership, Suzie Bailey.
Worse still, it’s the very staff who must deliver its reforms that the government has pissed off the most. The ‘social contract’ of NHS employment— basically, that we accept modest pay and difficult work in return for secure jobs, a career path and decent conditions—has been broken, especially for managers.
Repairing it needs to be at the heart of the ten year plan, not outsourced to another workforce plan, maybe, later this year. Maybe we do need a compelling vision after all—for why people should work for the NHS, particularly if they could offer their skills elsewhere. We can’t just rely on goodwill—because it’s more or less run out.
Related Stories
-

NHS job cuts: you’ll never walk alone
As the NHS redundancies in England loom, Rhys McKenzie explains how MiP will back you, and how members supporting each other and acting collectively is the best way to navigate this difficult process.
-

What now? Seven expert takes on the Ten-Year Plan
The government’s Ten-Year Plan for the NHS in England has met with enthusiasm and exasperation in equal measure. We asked seven healthcare experts to give us their considered view on one aspect that interests, excites or annoys them.
-

NHS job cuts: what are your options?
When politicians start reforming the NHS, there is only one certainty: some people will lose their jobs. But what options might be on the table and how does redundancy work? Corrado Valle explains.
Latest News
-

Government proposal for sub-inflation pay rise “not good enough”, says MiP
Pay rises for most NHS staff should be restricted to an “affordable” 2.5% next year to deliver improvements to NHS services and avoid “difficult” trade-offs, the UK government has said.
-

Unions refuse to back “grossly unfair” voluntary exit scheme for ICB and NHS England staff
NHS trade unions, including MiP, have refused to endorse NHS England’s national voluntary redundancy (VR) scheme, describing some aspects of the scheme as “grossly unfair” and warning of “potentially serious” tax implications.
-

Urgent action needed retain and recruit senior leaders, says MiP
NHS leaders are experiencing more work-related stress and lower morale, with the government’s sweeping reforms of the NHS in England a major factor, according to a new MiP survey.