Co-production: say it like you mean it
The NHS talks a good game on co-production, but many patients and carers still feel service changes are done ‘to’ them not ‘with’ them. As Jessica Bradley discovers, meaningful co-production means building lasting relationships and sharing decision making power.
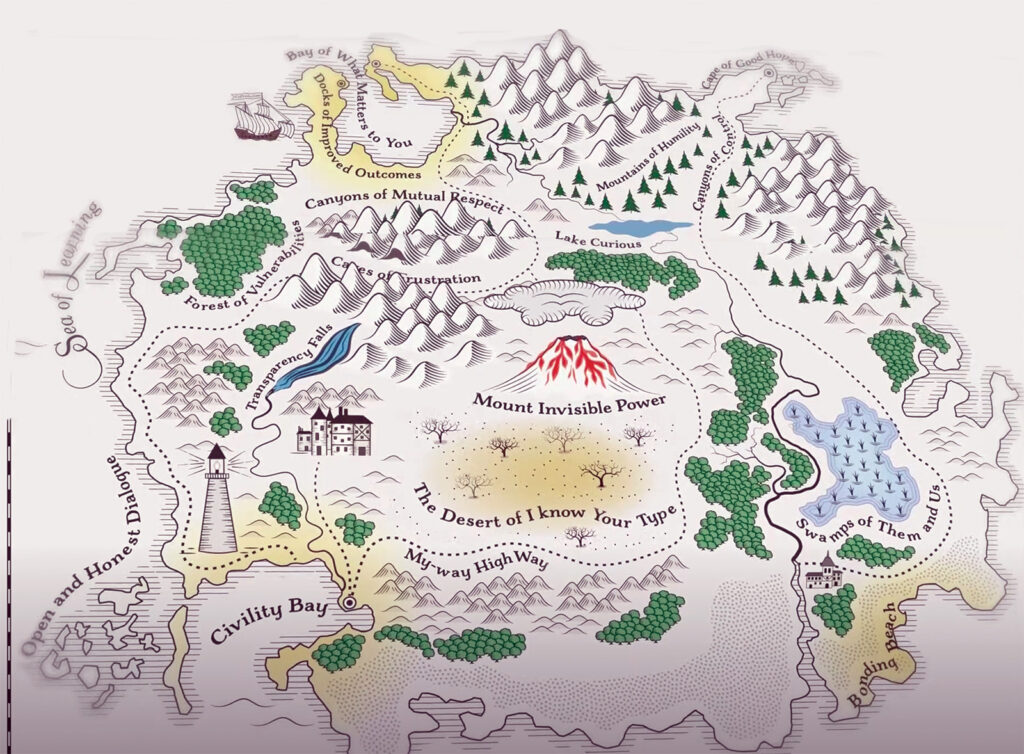
‘Co-production’ can be interpreted in many ways, but is generally understood as the process of consulting and including the public in designing and changing the services they use. The practice—which originated in the disability and mental health rights movements—advocates for an equal relationship between the people running services and those who use them.
While co-production can be applied to many NHS projects, including the design of new services and the reconfiguration of existing ones, the term is increasingly being prefixed with ‘meaningful’, in an attempt to move beyond what many see as performative efforts to apply the concept.
“Co-production is often seen as tokenistic because people suspect a decision was already made before engaging with the public,” says Dan Wellings, senior fellow at The King’s Fund. True co-production, he says, requires a different way of working. “It’s not a technocratic solution,” he says. “You have to let go and realise that the answers to some problems might not lie in the system, but in communities.”
Upfront and honest
There are four pillars to effective co-production, according to Isaac Samuels, chair of the National Co-Production Advisory Group and an advisor on co-production to several NHS bodies:
- sharing power to make decisions together
- building relationships and trust
- valuing all perspectives
- outcomes-focused action
To enable a “reasonable” conversation, Wellings says, the parameters within which the co-production team is working should be set early on. Staff must be upfront and honest with the co-production group about what can and can’t be co-produced, he explains, depending on the budget and other factors, and about what decisions have already been made.
“This might be a conversation about who’s best placed to provide services on mental health for young people,” he says. “The answer might not be the NHS provider, but a community organisation, for example.”
A group of researchers and family carers working with Warwick University recently collated their learnings into a ‘toolkit’ for co-producing research projects with family carers of people with a learning disability. The seven ‘golden rules of co-production’ they came up with are just as relevant to service providers, the team say.
Joanna Griffin, a psychologist and research fellow at Birmingham University, who worked on the project, says: “People talked about being brought onto a project at the end when everything has been decided already, which felt tokenistic. They emphasised the importance of having lived experience experts from the beginning.
“They also talked about wanting to feel like an equal partner in meetings, which includes not using jargon or acronyms, or people’s titles,” she adds.
The toolkit also highlights the need for researchers and service providers to be sensitive to the fact that people are often talking about difficult and personal subjects, and to not push them to talk beyond what they’re comfortable with.
Hard to reach
To effectively tackle health inequalities, services must also engage with people from minority ethnic communities or those living in the most deprived areas, who are often systematically excluded from decision-making processes, explains Wellings.
“Sometimes you know some groups will be disproportionately [more] represented than others, but if you’re really going tackle health inequalities, you need to engage the groups of people that services often refer to as ‘hard to reach’,” he says.
Isaac Samuels says experiencing ‘meaningful’ co-production felt like being an equal partner in shaping his own care. “At the individual level, co-production can be as simple as a clinician asking, ‘What works for you?’ rather than assuming they know,” he says.
“For me, that made all the difference when I was involved in a mental health project. Staff didn’t just consult me, they listened, adapted appointments around my life, and acted on what I said.”
Fiona Flowers is head of practice improvement at campaign and advisory group Think Local Act Personal and was the lead for developing Making It Real, a co-produced framework setting out the principles of good care, which is used by the Care Quality Commission and many other NHS organisations.
Flowers says the keys to effective co-production are trust, good relationships and a willingness to make mistakes along the way.
“If people know we’re coming from the right place, we can learn and improve together,” she explains. “A lot of the fear around co-production comes from people worrying about saying or doing the wrong thing, but at the heart of it, it’s really just about being human with each other—and that’s what people value most.”
Visible leadership
According to a review of research by NHS England, managers and leaders have a crucial role in the co‑production process. Leaders must ensure that co-production is systemic, and that requires culture change at strategic, operational and individual levels, explains Flowers.
“Visible leadership around co-production involves verbally championing it, and ensuring you’re providing the mechanisms and support in order for it to be a reality,” she says.
But existing cultures and ways of working within the NHS can make it difficult to embed meaningful co-production, warns Anthony Lawton, a consultant, former NHS manager, and author of Fit to Care—Insights From the Nursing Frontline. “Managers can be stuck, so we need to change that mindset of command and control into a flow process, and to focus on the patient—that’s missing,” he says. “Everybody thinks about their own silos, and what they need to do to tick their KPIs.”
This could explain why a lot of NHS work with the public revolves around feedback on existing services to check they’re working, rather than working with people on what services they need, Wellings says.
“Some leaders are very open about the fact that they have very little power to act because of the top-down initiative… they’re measured on waiting lists and targets rather than being held to account on meeting the needs of the local population,” he explains.
Co-production and the Ten-Year Plan

While there has been a shift in intention towards co-production in the NHS since the pandemic, the UK government’s Ten-Year Plan offers few concrete proposals on co-production, despite its emphasis on giving patients more control and bringing services closer to local communities.
The Plan leans heavily on expanding use of AI in the NHS, an area from which co-production has been notably absent so far. Research by the Health Foundation found that one in six patients actually think AI will make services worse.
This shows “a need to engage and involve communities in the roll-out to build support for the AI ambition”, argued Dr Natt Day (pictured), head of public involvement and engagement at UCL Partners, in a recent blog for the NHS Confederation.
In North-East London, Day is involved with a pilot of AI-screening technology and a phone-based clinical coaching service for patients at high risk of needing unplanned emergency care. “Throughout the project, we’ve involved local residents in developing the information materials, including the information about data and algorithm use, to provide transparency and build trust in the work,” Day explained.
Some of the new models of care being developed under the Ten-Year Plan, such as Neighbourhood Health Centres, seem fertile ground for co-production approaches, but they are not mandatory. The NHS Confed’s briefing on neighbourhood services says it’s “essential” that the development of new services is “community-led” and this “may” include co-produced service design (see: mip.social/copro-confed).
Co-production isn’t new, but how it should be embedded in NHS services is still being discussed and digested. There are some pockets of good co-production in the NHS, Wellings says, where people are fundamentally trying to change the way they work in a meaningful way. “But it still feels like the exception, rather than the norm,” he says. “Where this work is done really well, it can lead to genuine transformation in how services are provided.” //
Related Stories
-

Holyrood elections: Back from the brink—for more of the same?
After a big scare last year, the SNP are now clear favourites to extend their rule at Holyrood into a third decade, pointing to incremental reform rather than radical change for the NHS in Scotland. Rhys McKenzie reports.
-

Senedd elections: Tough choices, empty promises
As we enter 2026, the NHS in Wales faces some stark choices and a likely change of government. But the parties vying for power at Cardiff Bay will need to up their game to meet the challenges ahead. Craig Ryan reports.
-

NHS job cuts: you’ll never walk alone
As the NHS redundancies in England loom, Rhys McKenzie explains how MiP will back you, and how members supporting each other and acting collectively is the best way to navigate this difficult process.
Latest News
-

Job vacancy: MiP Assistant National Organiser
MiP is looking to recruit an Assistant National Organiser on a 14 month fixed term contract. Applications close: 4 March 2026.
-

FDA General Secretary Election 2026
Please find important information regarding the FDA General Secretary Election 2026 which MiP members may participate in.
-

Government proposal for sub-inflation pay rise “not good enough”, says MiP
Pay rises for most NHS staff should be restricted to an “affordable” 2.5% next year to deliver improvements to NHS services and avoid “difficult” trade-offs, the UK government has said.